8/26/2020
Patent Foramen Ovale (PFO)
Adapted from "Holes in the Heart," Stroke Connection Magazine, January/February 2011
A hole in your heart would seem to be the very definition of a "problem." Yet more than a quarter of the population has one, and for most it causes no adverse health effects. In fact, the vast majority of those affected don't even know it.
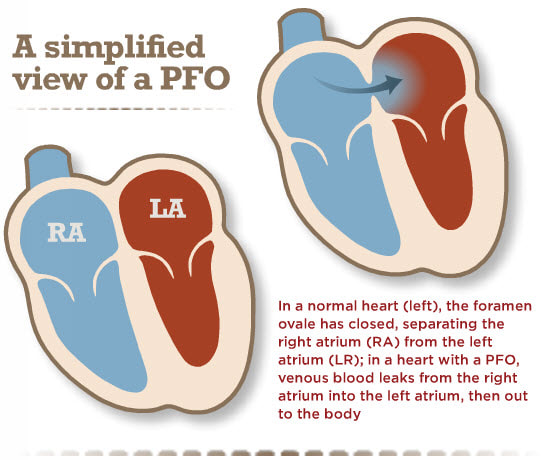
There are two kinds of holes in the heart. One is called an atrial septal defect (ASD), and the other is a patent foramen ovale (PFO). Although both are holes in the wall of tissue (septum) between the left and right upper chambers of the heart (atria), their causes are quite different. An ASD is a failure of the septal tissue to form between the atria, and as such it is considered a congenital heart defect, something that you are born with. Generally an ASD hole is larger than that of a PFO. The larger the hole, the more likely there are to be symptoms.
PFOs, on the other hand, can only occur after birth when the foramen ovale fails to close. The foramen ovale is a hole in the wall between the left and right atria of every human fetus. This hole allows blood to bypass the fetal lungs, which cannot work until they are exposed to air. When a newborn enters the world and takes its first breath, the foramen ovale closes, and within a few months it has sealed completely in about 75 percent of us. When it remains open, it is called a patent foramen ovale, patent meaning open. For the vast majority of the millions of people with a PFO, it is not a problem, even though blood is leaking from the right atrium to the left. Problems can arise when that blood contains a blood clot.
"Blood clots form in our veins all the time," said Dr. David Thaler, associate professor of neurology at Tufts University School of Medicine and director of the Comprehensive Stroke Center at Tufts Medical Center in Boston. "These are tiny blood clots of just a few millimeters that travel from all over the body into the vena cava where they enter the right upper chamber of the heart." From there they are pumped into the right ventricle, from where they enter the lungs. These tiny blood clots (individually called a venous thrombus) get filtered by the tiny capillaries in the lungs, after which the freshly oxygenated blood enters the left atrium, then the left ventricle. From the left ventricle, the blood is pumped out into the miles of blood vessels that feed oxygen and nutrients to every cell in our bodies. "Our lungs normally filter out these tiny clots, but a 2mm thrombus in the brain can cause real havoc," Dr. Thaler said.
That can happen when someone has a PFO or ASD. "PFOs don't actually cause strokes, but they provide a portal through which a thrombus might pass from the right to the left side of the circulation," said Dr. Patrick O'Gara, professor of medicine at Harvard Medical School and executive director of the Shapiro Cardiovascular Center. Depending on whether the clot takes a right or left turn as it exits the heart, it can travel to the brain and cause stroke or TIA. Statistically speaking, the odds of this happening are low, but it can happen.
How would you know?
Finding out whether you have a PFO is not easy, and it's something that isn't usually investigated unless a patient is having symptoms like severe migraines, TIA or stroke. Although the prevalence of PFO is about 25 percent in the general population, this increases to about 40 to 50 percent in patients who have stroke of unknown cause, referred to as cryptogenic stroke. This is especially true in patients who have had a stroke before age 55. In some cases, the PFO combines with another condition, such as atrial fibrillation, to increase the risk of stroke.
For survivors who don't have a definitive cause of their stroke, Dr. O'Gara suggests meeting with their neurologist to discuss the possibility of PFO. "There are many causes of stroke and having a PFO accounts for only a very small number," Dr. O'Gara said. PFO is diagnosed with an echocardiogram. An echocardiogram, also called a cardiac echo, creates an image of the heart using ultrasound.
What's to be done?
"The greatest myth about PFOs is that they must be closed. The vast majority of them require no treatment," Dr. O'Gara said. "If someone has one that is related to symptoms, they can be treated with aspirin, warfarin or catheter closure, depending on the circumstances."
Of course, drugs don't close the hole, "so the aim of drug treatment is to prevent a clot from forming in the first place," Dr. Thaler said. Nothing will close it except open-heart surgery or a closure device placed by a catheter threaded from the groin through the veins to the heart. Until recently, there were no approved catheter-closure devices designed for PFOs. The FDA has approved a device for patients who've had a stroke believed to be caused by a PFO, which reduces the risk of another stroke.
8/26/2020
Stroke - Life After a Stroke - Life After a Stroke
It can take weeks, months, or even years to recover from a stroke. Some people recover fully, while others have long-term or lifelong disabilities. A stroke team will work with you to manage your care. Your team may include specialists in neurology (brain, spinal cord, and nerves), rehabilitation, or mental health. You will also want to take steps to prevent another stroke and be aware of possible long-term complications. Call 9-1-1 if you have any signs of another stroke.
Healthy lifestyle changes
Heart-healthy lifestyle changes can help you recover from a stroke and may help prevent another one.
- Choose heart-healthy foods
- Aim for a healthy weight
- Manage stress
- Get regular physical activity
- Quit smoking
- Get enough good-quality sleep
Monitor your condition
It is important to get routine medical care after your stroke. Follow your treatment plan and talk with your doctor about how often you should schedule office visits.
- Talk with your doctor about the level of care you need. Some people return home after leaving the hospital. Others receive ongoing care at another facility.
- Take all medicines as prescribed. If heart-healthy lifestyle changes are not enough, your doctor may recommend medicine to control high blood pressure or cholesterol. Your doctor may also recommend aspirin or other medicine to prevent dangerous clotting that could lead to another stroke. Do not change the amount of your medicine or skip a dose.
Rehabilitation
After a stroke, you may need rehabilitation (rehab) to help you recover. Rehab may include working with speech, physical, and occupational therapists. Your care team may also recommend medicines to manage pain, muscle spasms, or other problems as you recover.
- Language, speech, and memory. You may have trouble communicating after a stroke. You may not be able to find the right words, put complete sentences together, or put words together in a way that makes sense. You may also have problems with your memory and thinking clearly. These problems can be very frustrating. Speech and language therapists can help you learn ways to communicate again and improve your memory.
- Muscle and nerve problems. A stroke may affect only one side of the body or part of one side. It can cause muscle weakness or paralysis, which can put you at risk for falling. Trouble using your hands, arms, and fingers is common, and training may help if you can no longer walk easily. Physical and occupational therapists can help you strengthen and stretch your muscles. They can also help you relearn how to do daily activities, such as dressing, eating, and bathing.
- Bladder and bowel problems. A stroke can affect the muscles and nerves that control the bladder and bowels. You may feel like you have to urinate often, even if your bladder is not full. You may not be able to get to the bathroom in time. Medicines and a bladder or bowel specialist can help with these problems.
- Swallowing and eating problems. You may have trouble swallowing after a stroke. Signs of this problem are coughing or choking during eating or coughing up food after eating. A speech therapist can help you with these issues. He or she may suggest changes to your eating plan, such as chopping up your food or drinking thick liquids.
Canes, braces, grab bars, special eating utensils, wheelchairs, and other devices can make it easier to keep doing your regular activities after a stroke.
Take care of your mental health
After a stroke, you may have changes in your behavior or judgment. For example, your mood may change quickly. Because of these and other changes, you may feel scared, anxious, and depressed. Recovering from a stroke can be slow and frustrating. Some people develop symptoms of post-traumatic stress disorder (PTSD).
Talk about how you feel with your healthcare team. Your doctor may recommend:
- Joining a patient support group, which may help you adjust to life after a stroke. You can see how other people manage similar symptoms and their condition. Talk with your doctor about local support groups or check with an area medical center.
- Medicines, such as antidepressants, or other treatments that can improve your quality of life.
- Support from family and friends, which can help relieve stress and anxiety. Let your loved ones know how you feel and what they can do to help you.
Prevent another event
Your doctor may recommend strategies to help prevent another stroke. This will depend on what caused your first stroke.
- Carotid endarterectomy. Your doctor may recommend this if you have carotid artery disease.
- Medicine or surgery for a heart condition. Blood thinners can help reduce the risk of another stroke due to atrial fibrillation. If you have a congenital heart defect that makes it easier for blood clots to travel to the brain, your doctor may suggest surgery to fix the problem.
If you recognize any signs of stroke, call 9-1-1 right away.
Learn the warning signs of serious complications and have a plan
The most common side effect of taking blood thinners to reduce your stroke risk is bleeding. This happens if the medicine thins your blood too much. This side effect can be life-threatening. Bleeding can occur inside your body cavities or from the surface of your skin.
Know the warning signs of bleeding so you can get help right away. They include:
- Blood in your urine, bright red blood in your stools, or black tarry stools
- Bright red vomit or vomit that looks like coffee grounds
- Increased menstrual flow
- Pain in your abdomen or severe pain in your head
- Unexplained bleeding from the gums and nose
- Unexplained bruising or tiny red or purple dots on the skin
Easy bruising or bleeding may mean that your blood is too thin. Call your doctor right away if you have any of these signs. If you have severe bleeding, call 9-1-1.
Syndicated Content Details:
Source URL: https://www.nhlbi.nih.gov/subscribe/3856
Source Agency: National Heart, Lung, and Blood Institute (NHLBI)
Captured Date: 2016-03-17 15:36:00.0
8/26/2020
Stroke prevention
You don't need to become a super athlete or go on a very strict diet to protect your heart and lower your risk of heart disease and stroke. Every woman can take steps every day toward a more heart-healthy lifestyle. And the best part is that being more heart-healthy also lowers your risk of other diseases like cancer and diabetes.
Get moving
For the most health benefits, you need to get enough aerobic activity to get your heart pumping and do muscle-strengthening activities every week. (Always check with your doctor before starting any regular exercise you are not used to doing.)
You should get at least 30 minutes a day of moderate-intensity aerobic activity, like brisk walking, on most days of the week. The 30 minutes of heart-pumping activity don't have to be all at one time. You can break it up into 10-minute activities throughout the day.
The Physical Activity Guidelines suggest that each week, women get at least:
- 2 hours and 30 minutes (150 minutes) of moderate-intensity aerobic physical activity, such as a brisk walk
OR
- 1 hour and 15 minutes (75 minutes) of vigorous-intensity aerobic physical activity, such as running
OR
- A combination of moderate and vigorous-intensity aerobic physical activity
AND
- Muscle-strengthening activities on 2 or more days
Learn more about how to be active for health.
Eat healthy foods
Making unhealthy food choices can lead to weight gain. But that is not the only risk. Unhealthy eating affects your arteries, blood pressure, glucose level, and many other parts of your heart health. Talk to your doctor or nurse about a heart-healthy eating plan that lowers your risk of heart attack and stroke.
Keep a healthy weight
Reaching and staying at a healthy weight will lower your risk of heart disease and stroke. If you already have heart disease, a healthy weight will help you control your disease and prevent heart attack. A slow and steady weight loss is the best way to lose weight and keep it off. Talk to your doctor about how much weight you need to lose and the best ways to do it. Learn more in our Healthy Weight section.
Know your heart disease numbers
Ask your doctor to check your blood pressure, cholesterol (total, HDL, LDL, and triglycerides) and blood sugar levels. Most insurance plans must cover these tests at no cost to you. These tests will give you important information about your heart health. Your doctor can tell you what your numbers mean and what you need to do to protect your heart.
Know the symptoms of heart attack and stroke
All women need to know the symptoms of heart attack and stroke and what to do. Make sure your friends and loved ones know how to recognize the symptoms too. If you think you are having a heart attack or stroke, call 911.
Knowing the symptoms and getting help quickly can help you survive a heart attack or stroke and make a full recovery.
Don't smoke
If you smoke, get the help you need to quit. Start by visiting women.smokefree.gov for woman-specific information, tips, and tools.
Limit your alcohol use
If you drink alcohol, do so in moderation. For women, this means no more than one drink per day.
"One drink" is:
- A glass of wine (5 ounces)
- A can of beer (12 ounces)
- A shot of liquor (1.5 ounces of 80-proof liquor)
If you don't already drink, don't start drinking for any reason. Moderate drinking is also linked to breast cancer, violence, and injuries. No amount of alcohol is safe during pregnancy.
Take care of yourself
Stress, anxiety, depression, and lack of sleep can raise your risk of heart disease. Take care of yourself with these steps:
- Get enough sleep. Most adults need seven to nine hours of sleep each night.
- Don't stress. Keep stress in check by taking time each day to relax and unwind.
- Treat mental health problems. Get help if you have trouble coping because of depression, anxiety, or other health problems.
- Make a well-woman visit. Make an appointment with your doctor for an annual well-woman visit.
Did we answer your question about heart disease and stroke prevention?
For more information about heart disease prevention, call the OWH Helpline at 1-800-994-9662 or check out the following resources from other organizations:
- Aspirin for Reducing Your Risk of Heart Attack and Stroke: Know the Facts — Information from the Food and Drug Administration
- ChooseMyPlate.gov — Nutrition information based on the 2015-2020 Dietary Guidelines for Americans
- Five Medication-Free Strategies to Help Prevent Heart Disease — Information from the Mayo Clinic
This content is provided by the Office on Women's Health.
Syndicated Content Details:
Source URL: https://www.womenshealth.gov/heart-disease-and-stroke/stroke/stroke-prevention
Source Agency: Office on Women's Health (OWH)
Captured Date: 2018-04-27 22:04:00.0
8/26/2020
Stroke symptoms
Strokes happen fast, and getting help quickly can help you make a full recovery.
What are the most common symptoms of stroke?
Stroke symptoms come on suddenly. The most common symptoms are:
- Numbness or weakness of face, arm, or leg, especially on only one side of the body
- Confusion or trouble speaking or understanding
- Trouble seeing in one or both eyes
- Trouble walking, dizziness, or loss of balance or coordination
- Severe headache with no known cause
What if stroke symptoms go away quickly?
Even if your stroke symptoms go away, call 911 right away. Temporary stroke symptoms are often caused by a "mini-stroke," or transient ischemic attack (TIA). A TIA happens when blood flow to part of the brain is blocked temporarily.
TIAs may not last long, but they still require treatment. Also, a TIA could be a sign that you are about to have a full stroke.
Did we answer your question about stroke symptoms?
For more information about stroke symptoms, call the OWH Helpline at 1-800-994-9662 or check out the following resources from other organizations:
- Know Stroke — The Know Stroke. Know the Signs. Act in Time. campaign from the National Institute of Neurological Disorders and Stroke (NINDS)
- Stroke Warning Signs and Symptoms — Information from the American Stroke Association
This content is provided by the Office on Women's Health.
Syndicated Content Details:
Source URL: https://www.womenshealth.gov/heart-disease-and-stroke/stroke/stroke-symptoms
Source Agency: Office on Women's Health (OWH)
Captured Date: 2018-04-27 23:48:00.0
8/26/2020
Stroke recovery steps
Stroke is a life-changing event. How long it takes you to recover depends on many factors, including the type of stroke you had, the area of your brain affected, and the amount of brain injury. The recovery process begins at the hospital as soon as you are medically stable. Often, this is within a day of having the stroke. Your doctor will talk to you about next steps. This will involve changes in your everyday habits, medicines, rehabilitation, or surgeries to lower the risk of another stroke.
Step 1. Educate yourself about stroke recovery.
The first step is to learn all you can about your condition and what to expect during recovery.
Ask your doctor, nurses, or physical or occupational therapist questions about your treatment and rehabilitation. Other stroke survivors can also help with practical tips. You can use the stroke resources on this website.
Step 2. Take steps to prevent another stroke.
If you've had a stroke, you're at high risk of having another. As you recover from your stroke, take steps to prevent a second one:
- Identify and control your stroke risk factors.
- Continue with your treatment plan. After a stroke, your doctor will work with you on a treatment plan. Your plan is designed to help you recover from your stroke and prevent another stroke. Even if you feel better, do not stop taking a medicine without talking to your doctor first.
Step 3. Figure out what rehabilitation services you will need.
Stroke rehabilitation is a program to help you recover from stroke. Almost all stroke survivors benefit from rehabilitation. However, many women do not join a rehabilitation program for reasons that are not clear. Many women are older at the time of their stroke and often go to assisted-living facilities or hospice after a stroke rather than to a rehabilitation program.1
Most insurance plans must cover stroke rehabilitation, although you may need to pay a copayment, coinsurance, and meet your deductible first. Find out what your insurance will cover, and what benefits you can receive from government programs or from your employer.
After a stroke, you will often recover some function in the first few months. This is part of the body's natural healing process. Women who get stroke rehabilitation:
- Relearn skills and abilities that were damaged or lost
- Regain as much independence as possible
- Learn to cope with any remaining limitations
Also, think about what, if anything, you will need from caregivers at home and what they are able to provide. Who is available to help with your care? How much time can they spend taking care of you? Can they provide financial support?
Step 4. Set goals for your recovery.
Set realistic, measureable goals for recovery in each area of your life your stroke affected. Keep in mind that stroke recovery is usually fast in the first few months. Then it may slow down. Having goals will help to motivate you to keep making progress.
Write down your long-term goals and create a timeline for achieving them. Break each one down into steps to make short-term goals.
Step 5. Follow through on your plan.
A stroke can often make you feel powerless. Part of recovery is figuring out how to live as independently as possible. Know that you are likely to face challenges as you adjust to the differences in how your body works.
The road to stroke recovery is often a long one, but focusing on your progress can help you reach your goals.
Did we answer your question about recovering from stroke?
For more information about recovering from stroke, call the OWH Helpline at 1-800-994-9662 or check out the following resources from other organizations:
- Find a Certified Stroke Center or Rehabilitation Facility — Directories of stroke and rehabilitation centers from the National Stroke Association
- Find a Neurologist — American Academy of Neurologists directory
Sources
- Petrea, R. E., Beiser, A. S., Seshadri, S., Kelly-Hayes, M., Kase, C. S., & Wolf, P. A. (2009). Gender differences in stroke incidence and post-stroke disability in the Framingham Heart Study. Stroke, 40(4), 1032–1037.
This content is provided by the Office on Women's Health.
Syndicated Content Details:
Source URL: https://www.womenshealth.gov/heart-disease-and-stroke/stroke/stroke-treatment-and-recovery/stroke-recovery-steps
Source Agency: Office on Women's Health (OWH)
Captured Date: 2018-04-28 00:07:00.0
8/26/2020
How is stroke treated?
The treatment you receive for your stroke depends upon the type of stroke you had and how quickly you receive medical care.
Treatment for ischemic stroke
The first-choice treatment for the most common type of stroke (ischemic stroke) is a clot-busting drug called tissue plasminogen activator (tPA, pronounced "T-P-A"). It is usually injected into one of your veins. This drug travels in the blood to your brain and breaks up the clot.
To work properly and safely, tPA should be given within 3 hours (but can be given up to 4 ½ hours) from the time your stroke started. In fact, the sooner tPA is given, the better it works. Before you can get tPA, you need to be tested to make sure you're not having a hemorrhagic stroke because tPA can make hemorrhagic strokes worse. This is why it is so important for a person having a stroke to call 911 quickly.
Some people with ischemic stroke can't get tPA. They might have gotten to the hospital too late or have another medical condition. These people will receive a different treatment:
- Blood thinners. These medicines can improve your blood flow if you have a clot. If you have atrial fibrillation or a history of stroke, your doctor might put you on long-term blood thinner treatment to prevent another stroke in the future.
- Blood clot removal. Some people do not get to the hospital in time to receive tPA, or they were given tPA, but it didn't work. The doctor may use a device to remove the clot causing the blockage.
Treatment for hemorrhagic stroke
Hemorrhagic strokes are very dangerous and have fewer treatment options. Treatment usually involves trying to control the bleeding and reduce pressure with drugs or surgery. The type of treatment you'll receive depends on what caused the bleeding and whether the bleeding is inside or outside your brain tissue. The main options are:
- Drugs to lower blood pressure. High blood pressure is the most common cause of a hemorrhagic stroke. Usually, in these kinds of strokes, there are tiny leaks in blood vessels throughout the brain. Lowering your blood pressure can help heal the leaks.
- Surgery to release the extra blood. A lot of bleeding in your brain can cause pressure inside your skull that can damage your brain. Doctors may make a cut in your skull to release some of the blood and lower the pressure.
- Surgical clipping. This procedure is used to treat a stroke caused by an aneurysm in your brain that has burst open. Surgeons cut into your skull and use a metal clip to close the blood vessel that has burst.
- Endovascular coiling. This procedure is also used to treat a burst aneurysm. It doesn't involve opening the skull, so it can be less risky than surgical clipping. It also takes less time to recover afterward. In this surgery, the surgeon puts a long, thin tube called a catheter through a small cut in an artery. He or she moves the end of it to the aneurysm and releases small metal coils into the aneurysm. A blood clot forms around the coils and stops the bleeding.
- Procedures to correct abnormal blood vessels. Some hemorrhagic strokes are caused by abnormally shaped blood vessels. If the problem is close to the surface of the brain, surgery can correct it. For problems deeper in the brain, surgeons can use a catheter inserted through the groin to enter the blood vessels, block abnormal connections, and stop the bleeding.
After stroke treatment, you might also need rehabilitation to recover from the damage the stroke did to your brain.
Sources
- Powers, W. J., Derdeyn, C. P., Biller, J., Coffey, C. S., Hoh, B. L., Jauch, E. C., … Yavagal, D. R., on behalf of the American Heart Association Stroke Council. (2015). 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 46(10), 3020–3035.
This content is provided by the Office on Women's Health.
Syndicated Content Details:
Source URL: https://www.womenshealth.gov/heart-disease-and-stroke/stroke/stroke-treatment-and-recovery/how-stroke-treated
Source Agency: Office on Women's Health (OWH)
Captured Date: 2018-04-27 23:58:00.0
- Author
- Write something about yourself. No need to be fancy, just an overview.
- Original ellagic acid research* from black walnut in 1968 showed many pharmacological effects in small animals such as anti-tumor, brain-protecting effect, analgesic, and tranquilizer like properties, antibacterial, anti-histaminic or anti-inflammatory effects, along with blood pressure-lowering action. Some of the experiments were so powerful that Ellagic acid prevented death almost 100% in mice from electroconvulsive shock and death from the acute release of histamine by strong histamine liberators similar to the prevention of mortality by acute anaphylactic like a shock.
Polyphenols are micronutrients with anti-prolific and antioxidant properties that can prevent prostate cancer, diabetes, and cardiovascular diseases. These health benefits were first discovered during the period 1977 - 1990 after the original ellagic acid (EA) research results were known as shown above. During this time, EA also became very popular on the internet as an anticancer compound. EA is found in many fruits, nuts, and vegetables, therefore easy to consume in vegan or vegetarian diets. Currently, there are more than 4000 publications & patents on ellagic acid supporting the above health benefits.